|
||||
|
Keeping Yiayia (Grandmother) at Home |
||||
The phone rang this morning quite early, a call from back home. At first we had thought that the mounting snow accumulation in New England had finally managed to wreak havoc with our property, but no. My cousin was calling to tell me that my elderly aunt had passed away. We knew that her health had been declining--and I had seen her only a short time before--but God called her to Him the night before last. It was perhaps a blessing, for with her serious heart disease, I knew what was waiting for her, having experienced it all with my father. |
||||
|
It was terribly sad for me. She was the last of 6 children born to my maternal grandparents who had settled in a New England textile-mill town. Unmarried, she had managed somehow to make her in-town duplex work for her, able to walk to the grocery store and to the nearby Greek Orthodox Church. She was the one in our family to take care of my grandmother until she passed away. My aunt learned how to give her injections when her diabetes couldn't be regulated at the end. With a little help from other family members like my mother, Yiayia received the very best possible home-care. But my aunt had been Yiayia's primary care-giver when declining health dictated more direct action. |
|
|||
|
|
||||
| There are actually many options open to elderly people who need extra help, apart from admission to nursing homes. There are assisted living facilities and day-care programs available, as well as personal care assistants and elder-sitters to offer help at home. Don't forget that family members, relatives and friends may be willing to help out. And in today's depressed economy, there are surely reliable helpers in your area who would be delighted to earn extra money by working with your parents or grandparents. Having good financial resources helps considerably, since the quality of private-pay home-care will nearly always trump public-pay home-care, but having only limited funds shouldn't deter you from exploring options. |
|
|||
Find a supportive physician The first task is to find a physician or nurse or physician's assistant who believes in the benefits of home-care and who will be on your side when you have to work against accepted norms in health care. You will have no greater ally. For without a competent, expert authority, your decisions concerning health care may be brushed aside by others, making your efforts doubly difficult. Interview physicians and staff. Find someone, preferably a gerontologist or internist with a sub-specialty in gerontology, who will help you assist your loved ones at home. My mother's physician also worked with nursing home patients and VA patients, a mark of his compassion as I had learned over the years. Without the physician's full support, I realized that it would have been next to impossible to keep my mother at home. For when she had spells with additional small strokes and dementia, there were times when she needed immediate, but unscheduled treatment; conversely, sometimes we just couldn't get her ready in time for appointments because her legs would give out or because she was having trouble with motor control. A couple of times, near the end, when she was completely bed-ridden, I wanted to nominate her doctor for a medal, because he offered to stop by the house to see her, knowing that we just plain couldn't transport her to his office, even with the Hoyer-lift, the transfer boards, the gait-belts, and strong home-aides. And no, the local "free" transportation for the elderly wouldn't have worked: they insisted on scheduling transportation far in advance, and would then make us wait hours to pick us up and hours at the doctor's office to return home. For someone with dementia and all that usually accompanies it, waiting hours simply wasn't an option. Likewise, my father had found several excellent physicians, a general practitioner and cardiologist whose doors were always "open," offering invaluable and timely care on many an occasion. Both were generally supportive of our efforts to help my father at home. So, my first piece of advice is to find a physician who encourages home-care. They exist. |
||||
Use assistive devices and equipment Second, explore all options for home modifications and assistive devices. Medicare will pay for many, if not all of these devices, whenever a physician writes that they are necessary. There will be additional paperwork for larger ticket items like wheel-chairs, hospital beds, lift-chairs, oxygen-producing machines, and motorized wheel chairs, but many vendors will help with the requisite paper-work or do it for you and send or fax it to the physician's office for review and signature. But there are even smaller items that may make a great difference in allowing Yiayia and Papou to carry out daily, but important tasks. For example, I searched far and wide on the Internet to find simple black plastic rings that snapped onto zippers, allowing my father to zip up his shirts and jackets. When he needed warm but comfortable shoes after he could no longer walk, we bought him pairs of thick suede slipper-boots with warm wool linings. After he lost the use of his fingers, we converted all door hardware to lever-style handles. For my mother, we began buying footed canes, then walkers, and eventually wheelchairs. Along the way, her bed acquired bed-canes, then full-sided bars. Long-handled grabbing tools made all the difference for them in reaching high items. Assistive telephones amplified voices and magnified numbers to allow them to make calls more easily. And when my mother started to fall--after my father had been relegated permanently to a wheel chair--we installed a Life-Alert phone line with bracelet button so that they could call for help quickly. These are just a fraction of the help-aids available to loved ones willing to expend a bit of time to research them and to find the best prices available. |
|
|||
Where to find devices and supplies Most areas have plenty of medical supply stores which can readily supply the most basic items, like canes and grabbing-tools. But I wasn't able to find any local store to offer the small plastic zipper-rings. These I discovered myself on the Internet (a company in California--about $3 for a bag of 6?) and ordered them. Likewise, when my poor mother became bed-ridden, we had to find adult "pull-up pants" for her, an adventure worthy of an entire chapter. But briefly (no pun intended), the best products were not offered locally; I had to order these (MoliCare brand products) from a specialty vendor in Illinois. For this brand worked better than anything else on the market at that time, including products offered at local medical supply stores, allowing us to keep her dry overnight without interrupting her sleep. And interestingly, Medicare wouldn't pay for this great product, only a terrible brand that was entirely ineffective. It was O.K. We paid out-of-pocket for the products that actually worked. So, shop at medical supply stores for the items that you need quickly (armed with a physician's prescription slip, including diagnoses and other necessary data), but search out online vendors for better and more cost-effective products. Keep in mind that on-line vendors may accept prescriptions for products and file claims for Medicare payment. For many years I ordered my mother's pills online (Drugstore.com) because they were much cheaper and the delivery was reliable, coming straight to the house. I used to order adult bibs online, too, as well as snap-secure garments because I couldn't find them anywhere else at the time. And periodically compare pricing for all products used, because some companies will offer specials or slash prices deeply to attract new customers or encourage repeat orders. But don't forget such large discount stores as Wal-Mart and Sam's Club where bulk items can be purchased. Eventually I picked up all of my mother's puddings, custards, and jello snacks there, reducing her costs. She absolutely loved the microwaveable, single-serving Spaghetti-O's, something that used to make us all chuckle. My father used to joke with the pharmacists at the local Sam's Club, all of whom knew him by sight, because they would help him get his prescriptions renewed and he could tool around their large store on a motorized cart while they got everything ready for him. On my end, I was pleased that his Sam's Club "system" worked well, because we were able to shop there while he was wheeling around. I always purchased a number of paper products and over-the-counter medications there at very competitive prices. Ramps for walkers and wheelchairs are indispensable for long-term home-care. We decided upon a portable, ADA-compliant, metal-mesh ramp from a specialty vendor because we didn't know how long we would need a ramp, if indeed one would help my mother at all. It soon became clear that it was a good decision because my father, too, began using the ramp, and even the aged family dog who had arthritis in her legs. But ramps come in many materials and sizes. There is one for every circumstance. Shop around. An inexpensive wooden one can even be built over an existing set of stairs and later removed. We were fortunate in that the town required us to obtain a permit for its installation; in return, the code officer inspected the ramp to ensure that it was indeed solid and ADA-compliant as promised. One elderly, unmarried relative didn't remain in her home, despite my encouragement, because she didn't want to install a stair lift to the second floor of her home or try to convert an unused first-floor dining room into a bedroom. She could have done either of these very easily if she had been supported emotionally by her closest blood relatives who lived far away. We had young cousins locally (more distant blood kin) with construction experience who could have guided her or overseen modifications. Her home was a lovely vintage cottage-style home that would surely have brought her a tidy sum from a reverse home mortgage, one sufficient to modify her living environment and to allow her to secure the help of home aides. Working in her favor was the fact that her home was not far at all from the center of the city (less than 5 minutes) and a nursing school at the nearby university branch. I kept trying to tell her that she could call the nursing program and ask to hire a nursing student, offering free room and board in return for a reduced rate on home-care. Her out-of-town young relatives didn't want to go along with it and even went so far as to tell me very politely to mind my own business. I offered all of the assistive devices and equipment accumulated by my parents, even the portable metal ramp, but they still became upset with me.Very sadly, my relative lived out the rest of her life, another 2 or 3 years, in a nursing home, with only annual visits from the out-of-town relatives. Because she was always so self-sufficient and hard-working it was heart-breaking to observe all of this, since in my heart I believed that it could have been better for her. (Αιωνία της η μνήμη.) Seek out helpful information from health-care providers, friends, and agencies Don't be afraid to ask questions of health-care providers, friends, and others, anyone who works regularly with the elderly. In many cases, they've been there before and already done it and will be happy to offer the benefit of their acquired expertise. In our case, I learned to my surprise one day that I should have been bringing my mother to a denturist for her dentures, not a dentist. So, I picked up the phone, made an appointment, and discovered that I was only going to pay a fraction of the cost to replace my mother's lost dentures. (We never did find out what happened to them.) At one point during the long and slow decline of my mother, when we had been about to give up, along came this perky little red-headed home-aide to tell us that we could still care for my mother at home. And she proceeded to tell us what we needed and taught us how to do it. We learned how to use Hoyer lifts and transfer boards. Our guiding star even showed us how to take care of bed-ridden patients. Her enthusiasm and can-do attitude earned my unstinted respect and gratitude. But she wasn't the only one who helped us. There were many who offered their knowledge generously. I bet that I must have learned something from every single one of the aides that helped us, each of them offering different talents. One showed me how to move my mother using the bed sheet. Another with advanced training showed us how to obtain and record blood-pressure readings. And yet another taught us the value of "fun" and "play" with my poor mother, a situation that required effort when her condition reached a nadir. She arrived singing at the beginning of her shift every day, uplifting all of us. In no time at all, my mother was singing right along with her and we were harmonizing, a human-wrought miracle. Local departments of health or human services may be able to put you in touch with valuable resources, whether they are governmental programs or simply the names of respected local home-care agencies. Don't neglect to ask for advice. In Maine, the Southern Maine Agency on Aging serves as a clearinghouse for information on helping the elderly. More than once I turned to them for information and advice, all of which proved useful. Adult day programs It was through a public-health nurse assigned by Medicare that I learned once about a day-program for seniors in a nearby town. Even though it was a small program at a local church, it was run by a professional who was also the pastor. I have to admit that I was skeptical at first, but Nurse Diane (who sadly passed away from lung cancer before we lost my mother), recommended it. When I hesitated, she said that she would be willing to bring my mother for a trial one afternoon and that she thought that the socialization would be good for her. O.K, I consented. And you know what? It was great. My mother just loved it. The group engaged in a number of different activities and had fun most of the time. And what's more, during the hours she was there, we didn't have to worry about her. We arranged for a taxi service to drop her off and pick her up initially, but when she needed more assistance, we all took turns with the transportation. Sometimes I would arrive early just so I could join in with the sing-along sessions of American golden oldies! Several years later, the program ended, to our disappointment, but the director recommended another similar day program in a town farther south. Shortly afterward we had my mother signed up for that and she was attending at least a few days every week. Since this second program was capable of offering more medical assistance than the previous one, she was able to participate for several more years until she needed full-time care. Attending an adult day-care was one of the critical factors that allowed us to keep my mother at home, since there were nurses on duty at the center who could dispense prescribed medications and the program was run by an experienced, licensed social worker. Sometimes I dropped in unexpectedly to observe or to participate; from what I could see it was a first-rate program that greatly helped my mother. There were a few unexpected side-benefits, too, in that the program administrators arranged periodically for outings for the entire group, and during my mother's last year, two other elderly Greek ladies who had been childhood friends also joined the program. Ask around and observe candidate programs yourself. Good programs will be run by certified personnel who will keep everything and everyone fastidiously clean and adhere to the strictest ethical and legal regulations, all while planning a range of activities to engage seniors. In some cases, transportation may be offered by the facility, especially if located close by. Some programs are designed to provide day activities for nursing home residents and take place in their facility, but others like the one my mother attended are independent programs housed in a different building elsewhere. We were billed hourly and invoiced monthly for my mother's participation, a great bargain considering what the staff accomplished for us. Home-aides and sitters If you decide upon home-care, eventually you will need to hire home-aides if you and your family can't provide round-the-clock care. You can hire them directly yourself, being sure to observe all regulations and laws, or you can contract with an agency to do so. You'll probably save yourself quite a bit of money through direct hiring, though, so don't shy away from trying it. Ask to see current certificates of CNA's/PCA's--the group that should be providing home care unless you need skilled nursing care, which might require LPN's or RN's. If you only need cooking, cleaning, laundry and the like, don't hire medical personnel; home-makers and elder sitters are always available to help with these chores, and at a much-reduced hourly rate. One option that might work for you is one that we employed: we worked out a combination of hourly rates, along with some secondary perks that the aides liked. In the case of our best home-aide--also a former CNA--we permitted her to babysit her grandson while watching my mother. She was thrilled to have the youngster at hand, saved a pile of money in baby-sitting/day-care costs, and my mother enjoyed having the tot around. Caution needs to be exercised here, though, because if your loved one is suffering from a depressed immune system or is very weak, it may not be advisable to have a toddler around. Check with a physician before embarking on a plan like this one. Other benefits we provided home-aides were lunches and ice-creams at local eateries, when my mother had still been somewhat mobile. We also paid them to do household shopping when we ran out of supplies, and compensated for the cost of the trip; aides could take care of their own household shopping at the same time. One weekend aide regularly brought her laundry to my folks' home, after asking our permission; since her work for us was essentially moon-lighting on a second job, we recognized that she wouldn't have much personal time to do her own laundry and household chores. It thus was an easy perk that we could offer to entice reliability. |
||||
Keeping a daily home-care journal One of the tools that helped us assemble a team of helpers and deliver good care was to keep a daily journal. Everyone who helped out--even if it was just to give my mother a snack--was required to write an entry in her journal. Name, date, time, and observations all appeared there. That way, if there was a problem with my mother's health, the in-coming helper could read up on her status. I used the journal, too, to point out changes ordered by the physician or modifications suggested by the principal aide. Sometimes we just wrote that everyone was having a great day and added a smiley face! But when we had to measure fluid build-up in her lower legs, her daily weight, or take her blood-pressure, we used the journal as a medical chart, recording everything in the daily entries. |
|
|||
Along with the journal, be sure to develop a home-care guide book, particularly if there are many people helping with care. This should include everything, from details of daily care and routines, to favorite foods, how to care for family pets, and phones numbers for emergencies. Ours was about 80 pages long, covering everything from service and utility providers, to the names and phone numbers of doctors and lists of all prescriptions. At the back we inserted copies of their medicare cards, supplemental insurance cards, and drivers' licenses in case they had to be transported by ambulance to a local hospital before we could return. A large 8x11 red-and-white magnetic page affixed to the side of the fridge had emergency numbers, too. Underneath that sign was a magnetic magazine holder with the guide-book. In a pinch, the helpers would be able to give detailed medical information, including all current major conditions and lists of medicines; without these, the work of the EMT's would be all the more difficult and aides might not be able to locate the data quickly. Putting Useful Technology to Work Advances in technology have recently helped to revolutionize health-care. We've all seen the miraculous advent of pace-makers and other such life-saving devices. My father benefited from some of these, using a motorized wheel chair with an oxygen-tank carrier. We all learned how to refill his oxygen tanks using a special machine delivered to his home. For these additional two or three years of life that the medical advances brought him, we were all exceedingly grateful. My father wanted to live and did whatever he had to do in order to keep going. At one point, his cardiologist arranged for special transmissions of cardiac measurements via telephony. I was amazed at this, not having realized that the technology formerly seen on television documentaries was now widely available to patients nationwide. |
||||
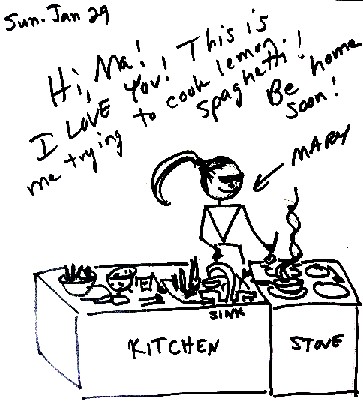
| Asking for and learning about the latest medical equipment is really only one facet of delivering home-care. "Low-tech" products also offer help, sometimes in unexpected ways. My parents had had a fax machine, now a relic from by-gone days, which I used regularly. Because my mother was extremely hard of hearing and had suffered from dementia, holding a piece of written correspondence in her hands allowed her to re-read the message frequently throughout the day. If she forgot what was in the message, she could read it again, reassuring her and keeping her occupied. Whenever I was out of the house for a large part of the day or away for a few days, I sent hand-written faxes to her frequently. Bold lettering in black magic marker told her how much I loved her and simple, hand-drawn images with captions showed her what I was doing. But the fax also worked to communicate with her doctors, home-care agencies and day-care program. While I was sitting with my mother, I was able to write up notes and sign forms, all delivered quickly via the fax machine. In between medical appointments, the fax became a means to transmit recorded data such as fluid retension, weight, and so on, helping her physician to monitor her condition more closely. |
|
|||
|
|
||||
|
(Posting date 12 May 2015) HCS encourages readers to view other articles and releases in our permanent, extensive archives at the URL http://www.helleniccomserve.com/contents.html. |
||||
|
||||
|
2000 © Hellenic Communication Service, L.L.C. All Rights Reserved.
http://www.HellenicComServe.com |
||||